Let’s say your navicular stress fracture wasn’t diagnosed for a year. A story that’s all too common.
If it were me or my kid I’d go for 8 weeks (sorry) of nonweightbearing (definitely in a boot as ankle movement rocks the joint where the stress fracture is) and crutches—trying NOT to touch the boot on the ground. Even for ‘little trips’ to the fridge etc. Light touch on the ground is OUT! 😊.
We’d check the navicular for tenderness at 6 weeks but definitely err on the side of caution (i.e. 8 weeks when the diagnosis was delayed). Then careful and skillful ankle and foot mobilisation and gradual return to activity over 3+ months. No quick fixes. Surgery definitely NOT faster.
Supersurgeon Joseph Torg published on this in 1982 and followed up with key papers over the next 30 years. That’s the 40 years I refer to in the title … 1982-2024.
An obvious question is: “When is the delay to diagnosis too long for conservative management to work?”. No-one has addressed that good question with research/data. But we’ve seen many athletes with 12-month delays (and more) who healed their fractures with nonweightbearing. (Khan et al., 1992)
What does surgery entail?
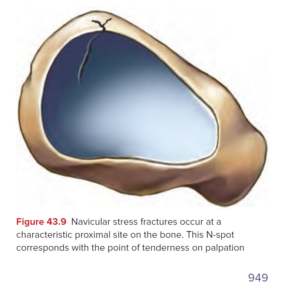
The point to realise about ‘surgery’ is that it’s not at all simple. If the surgeons suggest the ‘screw’ approach there are various ways of screwing a navicula. One screw or two? Remember, the goal is to compres a very small fracture (probably 3 mm in depth into the navicular, see picture) with a screw that may miss the fracture (depending on the surgeon’s approach, as above. In some cases of screwing, the screw is aimed ‘behind’ that fracture in the picture (distal to it)—the screw would not cross the fracture itself (too small). This is different to a scaphoid fracture screw where the screw crosses the fracture line and compresses the broken parts of that bone.
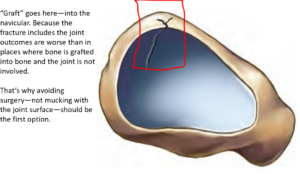
If the surgeons say they are going to do a “coffin graft” or some type of “graft”—putting new bone into the fracture site (from you or from a cadaver)—you have to realise that they are affecting the joint surface (where the talus fits into the navicular). So this new bone has to fit into a curved surface—of course, there is not going to be perfect healing. Once you say ‘joint’ you are saying risk of “arthritis”; risk of talonavicular arthritis (midfoot pain) with this surgery. (Sorry but it’s just the truth—what % of people?—Has not been well reported but I’d guess 20% of patients with grafts. I welcome correction/data here.
May I just add that I don’t believe the “98% success rate” for surgery in one of the studies you may see. I have heard of (and reported, Khan, AJSM, 1992) so many surgical failures that John McEnroe comes to mind … “surely you can’t be serious”. The authors are not lying—they are just reporting on a subgroup of patients; the surgeons who have more realistic results (I would say 60% success is good) don’t publish their results in a journal. Neither do surgeons who have even lower success rates of their surgery (and, I hope, give up on doing those very tricky operations and refer to superspecialists).
Paul Gasol’s NBA career was never the same after a navicular stress fracture. He had surgery. If we count that as a fail, we need to find another 49 NBA players who had successful outcomes of navicular surgery to reach that 98% number. Show me the money.
Michael Jordan managed his navicular stress fracture in 1985 without surgery. He was already playing for the Bulls–he made a wise choice. It’s all there in The Last Dance.
K2
PS: “Success” in this case (with nonweightbearing immobilization) would include some aching of the area with heavy activity for the first year at least after return to activity. But not the sharp pain. Being able to do everything but just knowing the foot isn’t the same as it was a few years ago or as the other side is a realistic outcome. “Occasionally grumbly” but knowing it’s stable/functional. “90%” instead of 100% would be success to me. What do you think?.
Here’s hoping this blog helps some patients and clinicians. Happy to amend bits that are wrong–it’s just a blog! Aiming to continuously improve. Kaizen. #PatientsFirst #HonestEvenIfItHurts
30th March update:
Thanks for a speedy reply from my good friend and internationally recognized foot and ankle specialist (and more) Dr Pieter D’Hooghe (MD, PhD). Chief Medical Office at Aspetar Orthopaedic and Sports Medicine Hospital, Doha, Qatar.
– if a nutcracker fracture (cuboid impaction) occurs, I need to fix it to support healing and avoid displacement.
– if you have a footballer who will be non compliant with 8-weeks of nonweightbearing immobilization, I stabilize and compress it percutaneously. (know your patient right? )
– I only open to put in a vascularized graft with fixation (that I learned from my vascular surgery colleagues – prior ultrasound guided branch detection ).

